BC Children’s Hospital Research Institute has found a way that kids’ immune systems might be able to be used to help fight off the most common type of childhood cancer.
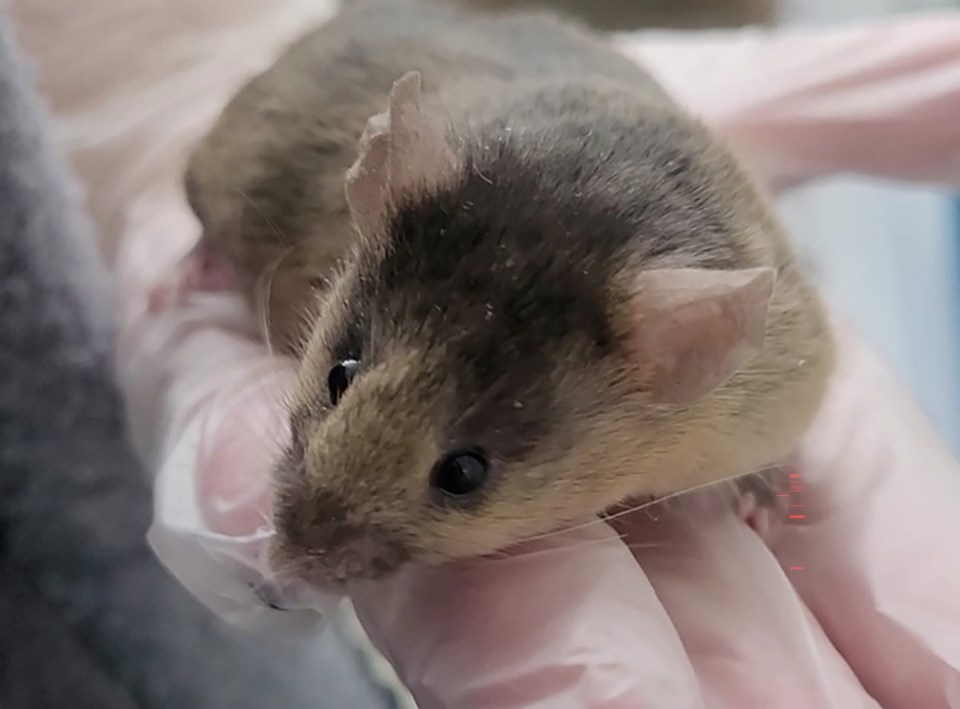
Researchers found that when infant mice were infected with a mild virus, their immune system kicked into action and those mice didn’t develop pediatric acute lymphoblastic leukemia.
This is a type of cancer that around 40 kids, usually between the ages of two and five, develop every year in B.C. Although most will be successfully treated, around one in 10 relapse, according to the BC Children’s Hospital Foundation.
This discovery was published last month in Blood, the flagship journal of the American Society of Hematology, as a “plenary paper,” which is the journal’s way of flagging it as a big deal. That sentiment was echoed by Amy Lee, an assistant professor of molecular biology and biochemistry at Simon Fraser University.
Lee was not involved with this study but does work with Tobias Kollmann, one of the study’s authors.
Researchers worked with infant mice, which were a couple of days old, and adult mice, which were around a month old.
These mice are bred to have an extra piece of DNA that causes a type of leukemia that looks very similar to a form of leukemia children get, says Gregor Reid, investigator at the Michael Cuccione Childhood Cancer Research Program at BC Children’s Hospital. Reid runs the lab where the study was done and is a senior author of the research.
The similarity between the cancers lets researchers look at mice to figure out what might happen with sick kids.
Both groups of mice were exposed to the mouse version of the cytomegalovirus, a common virus that kids usually catch while at daycare, Reid said. It’s a pretty mild infection and kids usually just get a runny nose for a couple of days, he added.
Researchers found that infant mice exposed to the virus were slower to get sick with cancer.
“Only mice infected with a virus very early in life were protected from developing leukemia,” Reid said. “We did not achieve the same result with adult mice, which suggests there is something unique about the immune system of newborns that makes this prevention possible.”
‘The direction future treatment is going in’
The immune system in infant mice isn’t necessarily fighting off leukemia cells, but is fighting off what are known as preleukemic cells, Reid said.
Preleukemic cells develop during fetal development and around five per cent of children are born with them, Reid said. A small percentage of them go on to develop childhood leukemia.
“One in 100 to 200 of the kids with preleukemia are getting leukemia,” Reid added.
Scientists don’t know why, Reid said, but they do know that preleukemic cells are a precursor to childhood leukemia, so “if you intervene and get rid of them, you could actually reduce the chances of that child getting leukemia.”
Ali Farrokhi, the study’s lead author, who led the research as part of his post-doctoral fellowship at the University of British Columbia, says that right now doctors can diagnose kids with cancer once they are sick, which limits what treatments you can offer them.
His research shows there may be ways to target preleukemic cells, which could mean that if a child is identified as having preleukemic cells at birth, doctors could closely monitor that kid and act much sooner if the cells start to develop towards leukemia.
“This is the direction future treatment is going in,” he said.
Farrokhi said researchers have been investigating the connection between viral infections and cancer since 1891. Early doctors would infect cancer patients in hopes that the virus might attack their cancer cells.
While that approach had some success, the risk was that patients could die from the infection, Reid said. When radiation was discovered as a treatment for cancer, the field started using that treatment and left viral infections behind.
Farrokhi said his research pinpointed that it was the timing of the infection, and not the virus itself, that was key to kicking the immune system into action to then attack the preleukemic cells.
“For mice you have to infect them within 10 days of being born in order to generate that protective immune response that depletes the preleukemia cells,” he said. Translating that into children, he said, the research “suggests that the first six months are the critical time for protection in children.”
Why infant intervention might be key
SFU’s Lee applauded the study for its thoughtful and thorough approach and its examination of how viral infections can both increase and decrease the likelihood of developing cancer. By looking at different ways cancer and the immune system react to infections, they were able to pinpoint something happening with the neonatal immune system, she said.
So what is it about an infant’s immune system that is so special?
The immune system goes through a radical development when it transitions from the sheltered in utero world to the wider world, which is just “laden” with pathogens, Lee said.
From birth to 28 days old, infants are at higher risk of dying from infections such as influenza and RSV, she said. This is not necessarily because the immune system is weaker during this neonatal period, but because it’s having to do a unique “balancing act” where the body has to respond to the exponential jump in exposure to pathogens without going “completely crazy,” because “too much inflammation will hurt the body too,” she said.
The immune system is “manic” during this time and goes through so many changes in the first couple of weeks. This is very different from the “stable” immune systems of adults, she said.
Reid said his team thinks it’s this neonatal window of time that’s providing the right conditions for the viral infection to stimulate the immune system to fight the preleukemic cells.
To be clear: Reid said he is not suggesting that we should infect babies with viruses, even mild ones, in order to protect them from cancer.
“But if we can understand this natural mechanism of protection, it could have implications for prevention, reduction of relapse rates or improved therapies because we know about an immune response that will get rid of those cells we want to get rid of,” he said.
Reid said this discovery isn’t necessarily unique to preleukemia, but that researchers were able to identify how the immune system normally and naturally changes as a child grows by paying attention to how the body fights off preleukemia cells.
The study says that this research could one day be used to create new cancer treatments or create preventive strategies to protect kids from acute lymphoblastic leukemia.
Currently, Reid said, kids with acute lymphoblastic leukemia are treated with chemotherapy, which will get between 90 and 98 per cent of patients into complete remission. Of those, 80 to 85 per cent will be cured by chemotherapy. But for 15 to 20 per cent of patients, the cancer will come back, “and for those we need treatment options,” Reid said.
Current treatments can have long-term effects because they target a wide range of cells and bodily functions. Researchers are looking for treatment options with fewer side-effects, Farrokhi said.
“I think what the study is showing us is that it’s possible to create an immune environment which is hostile to the leukemia,” Reid said. So if chemotherapy can eliminate 99.9 per cent of the cancer in a patient and “we could manipulate their immune system to make it inhospitable to those remaining leukemia cells, it might be a fairly innocuous way to increase cure rates and reduce the incidence of relapse.”
However, the research so far has identified how an infant’s immune system can be hostile to preleukemic cells, and most children who develop acute lymphoblastic leukemia are between the ages of two and five, which Reid said is a “challenge,” because these toddlers would have different immune systems.
Reid said they’d need to “see if this immune response that we’ve identified in neonates with preleukemia can be generated in older individuals with leukemia rather than preleukemia.”
“We’re seeing glimpses of being able to do that, but it’s a different challenge.”
Next steps
Once researchers can figure out what is happening with infants’ immune systems, they wouldn’t need to work with actual viruses, Reid said. They could take a piece or a protein from the virus that is not able to replicate and use that to stimulate the immune system.
This would be more like a drug used as part of treatment than a vaccine used to prevent the disease, he said.
Researchers additionally won’t know how the science translates between mice and humans until they are able to test human immune cells.
Reid said the next steps will use donated umbilical cord blood, which contains infant immune cells that can respond when exposed to a virus.
Farrokhi said they will also be running more experiments with mice to develop a slightly different type of pediatric leukemia and seeing what happens when they use different viruses too.
Farrokhi and Reid both requested that the work of their entire team and all the researchers at BC Children’s Hospital Research Institute be acknowledged for this discovery. They also thanked people who donate to BC Children’s Hospital Foundation who helped fund this research.
Those wanting to help out with this research are asked to consider donating their umbilical cord to science after giving birth.
Farrokhi said he will be looking for patients who develop childhood leukemia who previously had their umbilical cord donated. He will then be able to work with the previously donated tissue, which will have preleukemic cells in it, and see how those cells react to an infection.
Correction note: An earlier version of the article incorrectly said one in five patients who develop acute lymphoblastic leukemia will die. The article has been corrected to say one in 10 patients who develop acute lymphoblastic leukemia will relapse. One in five patients who are diagnosed with a childhood cancer will die.